World Sepsis Day (WSD) on September 13 is a global initiative to raise public awareness of sepsis, a leading cause of death and disability for millions of people every year. World Sepsis Day was introduced by the Global Sepsis Alliance, a collaborative effort led by various organizations at international level dedicated to increase the global knowledge of sepsis.
Sepsis – a global burden

48.900.000 people per year develop sepsis [10]
11.000.000 people die every year [10]
A study published in The Lancet in January 2020, estimate the global burden of sepsis in 2017 to be 48.9 million [95% uncertainty interval 38.9-62.9] incident cases and 11.0 million [10.1-12.0] deaths worldwide [10]. This is twice that thought previously [11] and is largely attributable to the far higher burden among people living in areas with a lower Socio-demographic Index (SDI), for whom data had previously been lacking.
Sepsis is associated with a high mortality
Mortality from sepsis and septic shock remains unacceptable high[1]. Patients with refractory septic shock, defined as requirement for dopamine >15 μg/kg/min or norepinephrine/epinephrine >0.25 μg/kg/min to maintain mean blood pressure above 65 mmHg present with a higher mortality [2].

Sepsis and COVID-19
It has been recognized that patients who are critically ill with COVID-19 have viral sepsis, despite some differences from sepsis caused by other pathogens. In addition, these patients frequently develop further bacterial infections (superinfections) which lead to a secondary septic status. Patients with severe COVID-19 suffer from multi-organ dysfunction, including acute respiratory distress syndrome (ARDS), vasodilatory shock, acute kidney injury, coagulopathy, and impaired brain, heart, and gastrointestinal function; similar to the clinical manifestations that characterize sepsis.
A systematic review has confirmed that COVID-19 causes death and disability due to sepsis: 85% of adults critically affected by COVID-19 develop sepsis, 40% of the whole spectrum of cases present with sepsis [3].
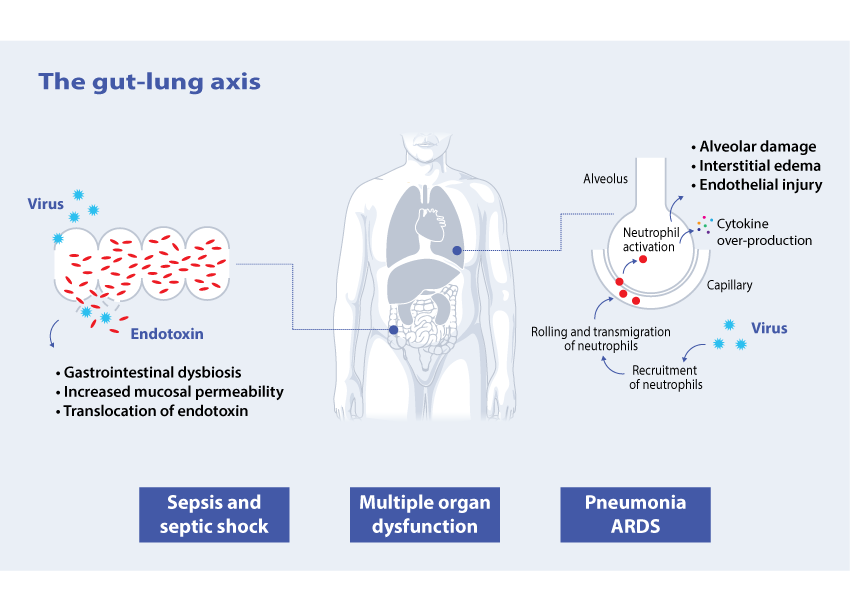
Pneumonia is the most common complication in COVID-19 patients. In severe cases this may be accompanied by a dysregulated immune response. Neutrophils have been found to play an important role as a generator of this response4 and rollling of neutrophils is one of the key factors in cytokine over-production [4].
Although coronaviruses are known as respiratory pathogens, they clearly have an ability to cross barriers and enter other organ systems [5]. One example of this is the gut-lung axis.
Up to 60% of COVID-19 patients have gastrointestinal symptoms at admission or developed during hospitalization and SARS CoV-2 viral RNA was found to be present in the faeces in 48% of patients [6]. Gastrointestinal dysfunction may lead to increased mucosal permeability and leakage of endotoxin [7]. High levels of endotoxin are found frequently in critically ill COVID-19 patients [8].
Patients who are hospitalized for extended periods in an ICU are more prone to superimposed infections [9], in addition to the primary viral infection. Gram-negative bacteria infection and/or direct mucosal gut translocation lead to the circulation of endotoxin (endotoxemia)[7].
The WHO resolution on sepsis
In May 2017, the World Health Organization (WHO) approved a resolution aimed atimproving prevention, diagnosis and cure of sepsis. The resolution calls for governments and policy makers to improve policies and procedures related to sepsis, with particular focus on prevention of infection and limitation of further spread of antibiotic resistance. The WHO stresses the importance of raising public awareness of sepsis through proper communication of symptoms, causes and possible outcomes.
References
- Shankar-Hari, M., et al., Developing a new definition and assessing new clinical criteria for septic shock: For the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA, 2016. 315(8): p. 775-787.
- Bassi, E., M. Park, and L.C. Azevedo, Therapeutic strategies for high-dose vasopressor-dependent shock. Crit Care Res Pract, 2013. 2013: p. 654708.
- Karakike, E., et al., COVID-19 as cause of viral sepsis: A Systematic Review and Meta-Analysis. medRxiv, 2020: p. 2020.12.02.20242354.
- Grommes, J. and O. Soehnlein, Contribution of neutrophils to acute lung injury. Mol Med, 2011. 17(3-4): p. 293-307.
- Openshaw, P.J., Crossing barriers: infections of the lung and the gut. Mucosal Immunol, 2009. 2(2): p. 100-2.
- Lin, L., et al., Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut, 2020. 69(6): p. 997-1001.
- Fink, M.P. and R.L. Delude, Epithelial barrier dysfunction: a unifying theme to explain the pathogenesis of multiple organ dysfunction at the cellular level. Crit Care Clin, 2005. 21(2): p. 177-96.
- Arunachalam, P.S., et al., Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans. Science, 2020. 369(6508): p. 1210-1220.
- Ronco, C. and T. Reis, Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nat Rev Nephrol, 2020.
- Rudd, K.E., et al., Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet, 2020. 395(10219): p. 200-211.
- Fleischmann, C., et al., Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am J Respir Crit Care Med, 2016. 193(3): p. 259-72.